In recent years, the field of obesity and cardiometabolic health has seen significant advancements, blending pharmaceutical innovation with lifestyle modifications to offer a more comprehensive approach to treatment. This integrated strategy promises not only better weight management but also improved overall health outcomes.
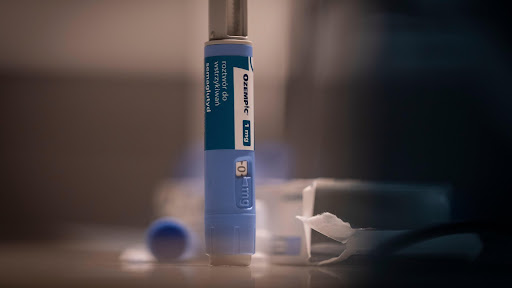
GLP-1 therapies are all the rage right now, and for good reason.
Several new studies highlight their incredible potential, and we’ll cover some of these groundbreaking findings in this blog. According to a recent white paper by Enara Health, integrating GLP-1 therapies into medical practices can significantly enhance patient outcomes while also adding a new revenue stream for healthcare providers. This dual benefit of improving patient health and supporting the financial health of medical practices is truly exciting.
To dive deeper into the benefits of GLP-1, let’s talk about how these therapies extend beyond weight management. Recent findings show that medications like Semaglutide and Tirzepatide reduce the risk of heart problems by 8%, with the most significant improvements occurring within the first year of treatment. This is especially promising for individuals with high blood pressure and diabetes, showcasing the multifaceted benefits of these medications.
But the perks of GLP-1 therapies don’t stop there. A Research presented at the ENDO 2024 conference reveals that semaglutide also enhances taste sensitivity in women with obesity, particularly for sweet foods. This change, linked to alterations in taste-related genes and brain responses, could make sweets less satisfying and promote healthier eating habits.

While GLP-1 therapy is already impressive on its own, there’s even more potential to unlock. New research indicates that combining GLP-1 therapy with other medications like bupropion/naltrexone can further boost weight loss, especially for those who initially don’t respond well to GLP-1 alone. This underscores the importance of personalized treatment plans, where different patient responses guide the choice of medications for optimal results.
However, a concerning trend has emerged: the use of unlicensed compounded GLP-1 peptides due to shortages. According to Dr. Lydia Alexander, these DIY alternatives pose significant health risks as they are unregulated and potentially dangerous. This highlights the critical need for professional supervision when obtaining and using these medications.
Parallel to these developments is a shift in how we measure obesity.
Traditional metrics like BMI are being challenged by new research advocating for the use of percent body fat (%BF) as a more accurate indicator of health. For men, 25% body fat now defines “overweight,” while 30% signifies “obesity.” For women, these thresholds are 36% and 42%, respectively.
Complementing this shift in metrics is the crucial role of exercise in obesity management. Recent research shows that combining aerobic and resistance training significantly boosts heart health by improving lipid profiles and reducing inflammation. This connection between body fat measurement and exercise underscores the necessity of a treatment model that balances medical interventions with lifestyle changes, including regular physical activity.
But medications and lifestyle modifications are not the only game-changers in weight loss—we have bariatric surgery too!
A recent study highlights that procedures like SR-LRYGB and LSG significantly reduce the need for diabetic and heart medications. For instance, SR-LRYGB cuts the need for diabetes medications by 79%. However, it also shows an increase in the need for psychiatric medications post-surgery, emphasizing the necessity for comprehensive mental health support alongside physical health interventions.
As we weave together these strands of medical innovation, lifestyle modifications, and technological advancements, a clear picture emerges: the future of obesity and cardiometabolic health lies in a holistic approach. By integrating medications, mental health support, dietary changes, and regular exercise, we can achieve sustainable health outcomes and improve the quality of life for individuals struggling with obesity.
For more insights and to stay updated on the latest developments, follow us on our social channels:
LinkedIn | Twitter/X | Instagram
Join us in embracing this holistic approach and transforming the landscape of obesity care.